| |
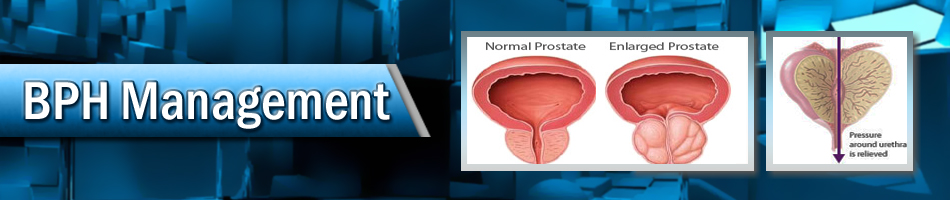
| BPH: Management (Benign Prostatic Hyperplasia/Enlarged Prostate) |
| |
| |
| What is BPH/LUTS? |
|
|
Benign prostatic hyperplasia (BPH) is a common urological condition caused by the non-cancerous enlargement of the prostate gland as men get older. As the prostate enlarges, it can squeeze down on the urethra. The symptoms associated with BPH are known as lower urinary tract symptoms. This can cause men to have trouble urinating and leads to symptoms of BPH. The symptoms associated with BPH are known as lower urinary tract symptoms (LUTS) |
| |
|
Diagnosis of BPH/LUTS |
|
|
As a man ages, his prostate may become larger and start to cause urinary symptoms and other problems. But what are some of those problems? How will a man know if he has an enlarged prostate (also known as BPH)? When should a man see his doctor? What kinds of tests will my doctor perform? The following guide should help answer your questions and help you make an informed decision about what your next steps should be.
|
| |
|
| What is the prostate? |
|
|
 |
The prostate is part of the male reproductive system; it is about the size and shape of a walnut normally and weighs about an ounce. It is located below the bladder and in front of the rectum, and surrounds the urethra, the tube-like structure that carries urine from the bladder out through the penis. The main function of the prostate is to produce fluid for the semen. |
|
| |
|
| What are the risk factors for BPH? |
|
|
Risk factors for developing BPH include:
» Obesity
» Lack of physical activity
» Erectile dysfunction
» Increasing age
» Family history of BPH
|
| |
|
| What are the symptoms associated with BPH? |
|
|
Since the prostate is just below the bladder, its enlargement can result in symptoms that irritate or obstruct the bladder. Common symptoms are:
• the need to frequently empty the bladder, especially at night.
• difficulty in beginning to urinate
• dribbling after urination ends.
• decreased size and strength of the urine stream
• sensation that the bladder is not empty, even after a man is done urinating,
• inability to postpone urination once the urge to urinate begins
• Pushing or straining in order to urinate.
In extreme cases, a man might not be able to urinate at all, which is an emergency that requires prompt attention.
Fill out the AUA Symptom Score and share the results with your health care provider.
|
| |
|
| How is BPH diagnosed? |
|
|
In order to help assess the severity of such symptoms, the American Urological Association (AUA) BPH Symptom Score Index was developed. This diagnostic system includes a series of questions that ask how often the urinary symptoms identified above occur and the amount of bother from these symptoms. This helps measure how severe the BPH is — ranging from mild to severe.
When a doctor evaluates someone for possible BPH, the evaluation will typically consist of a thorough medical history, an examination of the urinary sediment (urinalysis) a physical examination (including a digital rectal exam or DRE), and use of the AUA BPH Symptom Score Index. In addition, the doctor will generally do a urine test called a urinalysis. There are a series of other studies that may or may not be offered to a patient being evaluated for BPH depending on the patient’s current medical condition. These include:
• prostate specific antigen (PSA) - a blood test to screen for prostate cancer
• urinary cytology - a urine test to screen for bladder cancer
• a measurement of post-void residual volume (PVR), the amount of urine left in the bladder after urinating
• uroflowmetry, or urine flow study, a measure of how fast urine flows when a man urinates
• cystoscopy - a direct look in the urethra and/or bladder using a small flexible scope
• urodynamic pressure-flow study - tests the pressures inside the bladder during urination
• ultrasound of the kidney or the prostate – to view the enlargement |
| |
|
| When should I see a doctor about BPH? |
|
|
|
A man should see a doctor if he is bothered by any of the symptoms mentioned previously. In addition, he should see a doctor immediately if he has blood in the urine, pain with urination, burning with urination or is unable to urinate. |
| |
|
| What are some of the medical treatments available for BPH? |
|
|
Watchful Waiting/Active Surveillance
This treatment option is good for patients who have mild symptoms of BPH or have moderate to severe symptoms but are not bothered by their symptoms. Patients suffering from kidney problems as a result of BPH, urinary retention (suddenly being unable to urinate), or frequent urine infections, and urinary incontinence are not good candidates for this treatment option.
During watchful waiting, a patient is closely monitored by his physician but he does not receive any active treatment. Many patients’ symptoms can be controlled and/or managed by changing their current medications and diet. Patients will be examined yearly, and findings from the tests will be used to determine if additional treatment is needed in order to control a patient’s BPH.
The risk of watchful waiting may be that the patient’s symptoms cannot be reduced after active treatment is started.
|
| |
|
| Medical Therapies |
|
|
Alpha blockers:
These drugs, originally used to treat high blood pressure, work by relaxing the smooth muscle of the prostate and bladder to improve urine flow and reduce bladder outlet obstruction. Although alpha blockers may relieve the symptoms of BPH, they usually do not reduce the size of the prostate. They are usually taken orally; once or twice a day and work almost immediately. Commonly prescribed alpha blockers include:
• alfuzosin
• terazosin
• doxazosin
• tamsulosin
All of these drugs have the same equal level of effectiveness and side effects. Side effects can include headaches, dizziness, lightheadedness, fatigue and ejaculatory dysfunction. These medications are beneficial for patients who have bothersome to moderate severe BPH.
Patients who are undergoing cataract surgery may be advised by their physician against taking this medication until after their surgery.
5-alpha-reductase inhibitors:
Finasteride and dutasteride are oral medications used to treat BPH. In select men, finasteride and dutasteride can relieve BPH symptoms, increase urinary flow rate and actually shrink the prostate though it must be used indefinitely to prevent symptoms. Studies suggest that these medications may be best suited for men with relatively large prostate glands. These drugs reduce the risk of BPH complications such as acute urinary retention (suddenly being unable to urinate) and the eventual need for BPH surgery. Side effects generally are sexually related and include: erectile dysfunction decreased libido and reduced semen released during ejaculation.
Finasteride should not be used if men do not have prostate enlargement. Finasertide has been shown to cause more adverse effects in the beginning of its use; however, over a period of time the side effects between finasteride and dutasteride become equal.
Combination Therapy:
The use of both alpha blockers and 5-alpha-reductase inhibitors have shown to be superior to single drug therapies in men with larger prostates. The combination approach prevents the progression of disease and improves bothersome symptoms. However, this improved benefit may be associated with more side effects (possible side effects from both medications).
Anticholinergics: Another medical therapy that is an appropriate and effective treatment alternative for the management of symptoms related to BPH.
Complementary and Alternative Medicines/Phytotherapies:
These compounds, also know as herbal therapies, are very popular self treatment remedies. Currently there is no dietary supplement, complementary alternative medicine or therapy that is recommended for the management of BPH. Furthermore, the quality and purity of these over-the-counter supplements are not rigorously monitored, adding further uncertainty about the value and safety of these products.
Saw palmetto one of the more popular dietary supplements used by men has been shown to provide no benefit over a placebo for the treatment of BPH conditions and LUTS.
Minimally Invasive Therapies
Since the advent of medical therapy for symptomatic BPH with 5-alpha reductase inhibitors and alpha-adrenergic blockers, the need for immediate surgical intervention in symptomatic prostatic obstruction has been reduced substantially. However, alpha-blockers do not modify prostate growth, and even the use of prostatic growth inhibitors such as finasteride or dutasteride often fails to prevent the recurrent LUTS of BPH and urinary retention. In the past, these patients would almost certainly have undergone more invasive treatment earlier in the disease process.
Transurethral needle Ablation (TUNA) of the prostate
This outpatient treatment requires a urologist to insert a cystoscope-like device into the prostate. Each needle in the prostate emits low-level frequency radio waves that is sufficient to create a heat that kills the prostate tissue. The dead tissue from the prostate is absorbed by the body. The reduction in the size of the prostate alleviates the symptoms caused by BPH.
In the short term it is a very effective treatment however for long-term treatment patients may need to be retreated for their symptoms. In addition to the issue concerning the long term effectiveness of the treatment, finding the right candidates for the procedure has proven to be a challenge to doctors and is not consistent. One of the advantages of this treatment over others is the minimal sexual side effects short term.
Transurethral Microwave Thermotherapy (TUMT)
TUMT is a minimally invasive treatment that uses high-frequency radio waves to cause thermal injury to the prostate while providing relief for bladder obstruction. This treatment has been advanced in the last couple of years with new higher energy devices creating better long term outcomes. Yet, the advancement has done little to reduce the greater adverse outcomes that are generally associated with this treatment options.
Surgical Techniques
There are many surgical procedures to treat BPH. Surgery is the most invasive approach and is typically reserved for patients suffering from moderate-to-severe BPH related LUTS or complications which arise from BPH (e.g. urinary retention, progressive LUTS, recurrent urine infection). It is generally reserved for patients who have not been able to successfully treat the condition with other treatment options or for those who present with moderate to severe BPH.
The following are the generally accepted surgical treatment options:
• Transurethral resection of the prostate (TURP)
Has excellent outcomes and is the gold standard. All treatment options are generally compared to this approach. It is not safer with bipolar TURP meaning less risk of water intoxication leading to low sodium levels.
• Open prostatectomy
This surgery involves the removal of the inner portion of the prostate via a suprapubic or retropubic incision in the lower abdominal area. It is reserved for men with significantly enlarged prostate glands. The major risks associated with this treatment are the potential blood loss, need for transfusions, and a longer hospital stays. Outcomes are generally very effective with this approach in these patients.
• Transurethral holmium laser ablation of the prostate (HoLAP)
• Transurethral holmium laser enucleation of the prostate (HOLEP)
• Holmium laser resection of the prostate (HoLRP)
• Photoselective vaporization of the prostate (PVP)
• Transurethral incision of the prostate (TUIP)
• Transurethral
• Transurethral vaporization of the prostate (TUVP)
Before deciding if any of these treatment options are best make sure to discuss with your physician the following:
• Current symptoms and bother from these symptoms
• Size of prostate
• The potential benefits and risks associated with any form of treatment including watchful waiting
The following are things a patient should consider before deciding on a particular option:
• presentation (symptoms and how they feel about those symptoms)
• Size of prostate
• Surgeon’s experience
• Discussion with physician about the potential risks and benefits
|
| |
|
|
| |
|
|
 |
Endoscopic removal of urinary stones: PCNL, URS, RIRS, CLT |
|
 |
Lithotripsy (ESWL) |
|
 |
LASERS for stones and Prostate |
|
 |
Monopolar and bipolar TURP |
|
 |
HOLEP |
|
 |
Urodynamics and uroflowmetry |
|
 |
Laparoscopic urology surgeries |
|
 |
Paediatric urology surgeries |
|
 |
Urinary incontinence surgeries |
|
 |
Surgeries for genitourinary cancers |
|
 |
Reconstructive urology |
|
 |
Microsurgeries for infertility and impotence |
|
| |
|
| |
 |
| |
|
| |
| |
| |
| |
| |
| |
| |
| |
| |
|